Blood tests: which ones to get and what the heck do they mean?
Most people have had blood tests taken but the majority don’t know what they mean. I've asked countless patients about their results for diabetes testing, kidney, liver function and lipids panels and many wouldn’t have a clue what they’ve had done or what the results mean apart from saying their GP said “they were OK”…. or not. Personally, I don’t think that's good enough. Those test results are yours and it should be your responsibility to know what they are and what they mean and if you don’t know, ask. You cannot take charge of your health unless you know what is actually going on. It’s possible your GP or physician may be too busy to give you a full explanation, so in this post I will try to explain what tests to look at and what the numbers mean in relation to your metabolic health. It is also likely that your doctors may not know what exactly to look for so this will act as a primer for you to be well informed, maybe even better than your doctor.
So if you’ve been playing along at home and had your bloods done that I mentioned in my second post we’ll go through the results now as well as a few other tests:
Fasting insulin
Fasting glucose
HbA1C
Liver function tests
Lipids/Cholesterol panel
Kidney function
hsCRP
Ferritin
Vit D level
Thyroid function
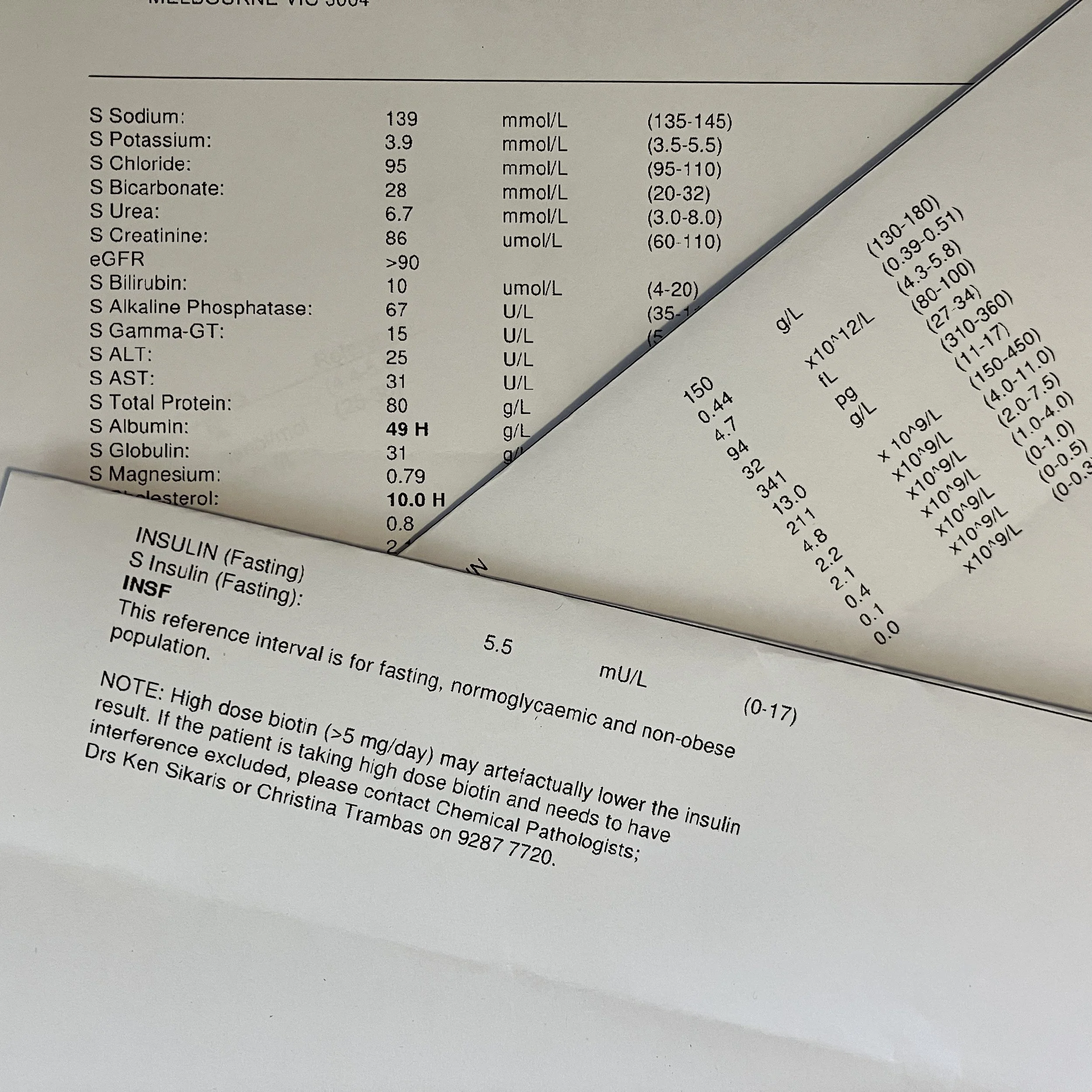
Fasting Insulin level: Quoted normal level 2-12
This is probably the most important test of your metabolic health that you can easily get done. Without knowing what your insulin level is, you really have little idea about where you stand on the spectrum from good metabolic health with insulin sensitivity to some degree of insulin resistance to overt prediabetes. The “normal” level for insulin is quoted to be anything up to 12. This level is obtained from looking at the average population and seeing what the fasting insulin level is in most people. As I've previously mentioned, if most people are metabolically unhealthy, then it's likely that they will have an elevated insulin level. This means that the normal levels for a population on average are falsely elevated.
For good metabolic health, that is when you are insulin sensitive - meaning your body responds appropriately to insulin - you should be aiming to have your fasting insulin level less than 7. If your insulin level is higher than this, it means that you are requiring more insulin in your body to produce the effect of keeping your blood sugar levels stable even when you’re not eating (fasted state). Think of it like this. If you drink alcohol consistently at a high level your body becomes used to it and over time it needs more and more alcohol to produce the same intoxicating effect. Our bodies in effect are becoming more and more resistant to the effects of alcohol. Similarly, with more and more insulin being produced by the pancreas in response to a high carbohydrate diet our bodies are gradually becoming resistant to the normal effects of insulin and require increasing amounts to produce the same blood sugar lowering effect. This means that you now have insulin resistance - a state where insulin isn’t producing the same result as earlier and more insulin is required. The problem here is that with time, more and more insulin is required to keep blood sugar levels in the normal range as the body becomes more and more resistant to its effects. This increased insulin level then leads to conditions such as diabetes, heart disease, obesity, polycystic ovarian syndrome, some cancers and poor lipid markers.
PLEASE NOTE: Just because you think you’re skinny or normal weight doesn’t mean that you can’t have high insulin levels. So everyone needs to have this checked as it may be one of the indicators that you are a TOFI (thin outside, fat inside) and at high risk for diabetes, no matter what your age, cultural background or gender.
Knowing what your insulin level is can help predict your chance of developing diabetes in the future, possibly up to 10-15 years in advance and if it's elevated above 7 then you can do something about it to prevent the progression to full blown diabetes.
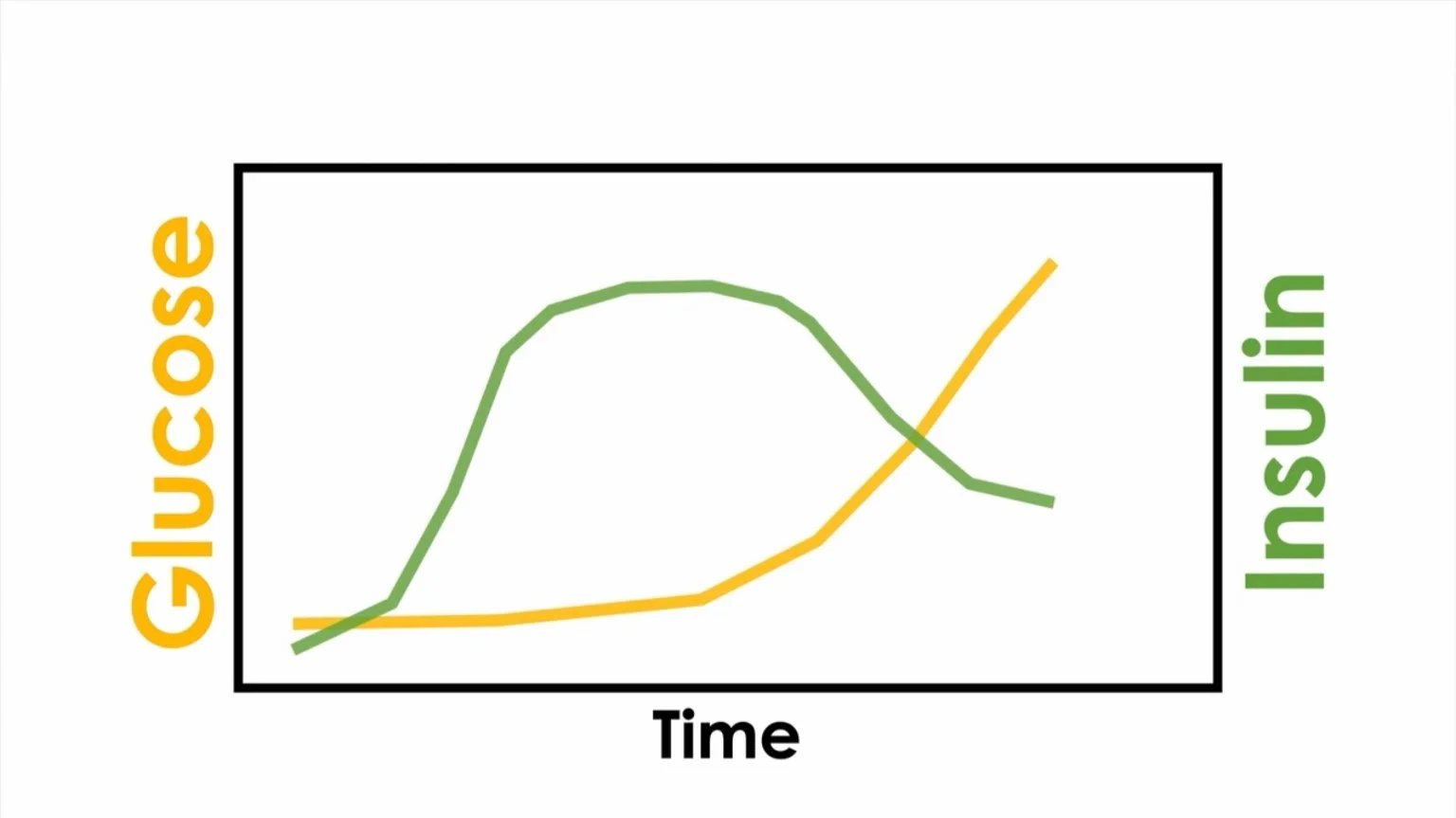
Glucose in yellow stays normal for 10-15 years while Insulin in green is already increasing. Only after many years of high insulin levels and the development of insulin resistance does the blood glucose start to rise at which point mainstream medicine makes a diagnosis of type 2 diabetes. However testing for fasting insulin can diagnose early insulin resistance and appropriate steps can be taken at this point to reverse this.
Image courtesy Why We Get Sick, Benjamin Bikman, PhD